Before being widely implemented, Mammography screening was tested in randomized controlled trials in the 1960s to 80s. Meta-analyses of these trials showed a relative reduction in deaths from breast cancer of between 15% and 25% among women aged 50 to 69, but these studies only compared Mammography to doing nothing. Compared to doing nothing, Mammography does save lives, but not when compared to a doctor doing a Physical Breast Exam.
It wasn’t until the Canadian National Breast Screening Study finally got it right and compared Mammography to a doctor doing a Physical Breast Exam that the truth began to be revealed. The original Canadian National Breast Screening Study, conducted 25 years ago, showed that Mammography did NOT reduce breast cancer mortality after 7 years.
In April 2014, the latest Canadian National Breast Screening 25 year followup Study again compared Mammography to Physical Breast Exam in women aged 40 to 59. The results were similar:
The Canadian Study Conclusion states, “our data show that annual mammography does not result in a reduction in breast cancer specific mortality for women aged 40-59 beyond that of physical examination alone or usual care in the community. The data suggest that the value of mammography screening should be reassessed.”
According to this 25 year prospective study of 90,000 women, physical breast exams are just as effective as Mammography at detecting Breast Cancers but without the harm from radiation and overdiagnosis and over treatment, including mastectomy, radiation, chemotherapy and the consequent emotional stress caused by routine annual mammograms. (British Medical Journal BMJ 2014;348:g366)
US only Nation still Recommending Mammograms for Women Age 40+
Only the US still recommends that women start getting annual mammograms at age 40 and continue into their 70’s. In Canada, the Canadian Task Force on Preventive Health Care does NOT recommend annual Mammogram Screening for women ages 40-49, and only recommends screening every 2-3 years for women ages 50-74. In Europe, except for the U.K. and Switzerland, women are told not to start getting Mammograms until age 50 and only get them every 2 years. In the U.K., Mammography starts at age 50 and women are told to only get a Mammogram every 3 years. In Switzerland, they finally got it right! The Swiss Medical Board has now stopped all new Mammography screening programs and is phasing out all existing Mammography programs altogether (published online April 16, 2014, in the New England Journal of Medicine).
Mammography’s Fatal Flaws
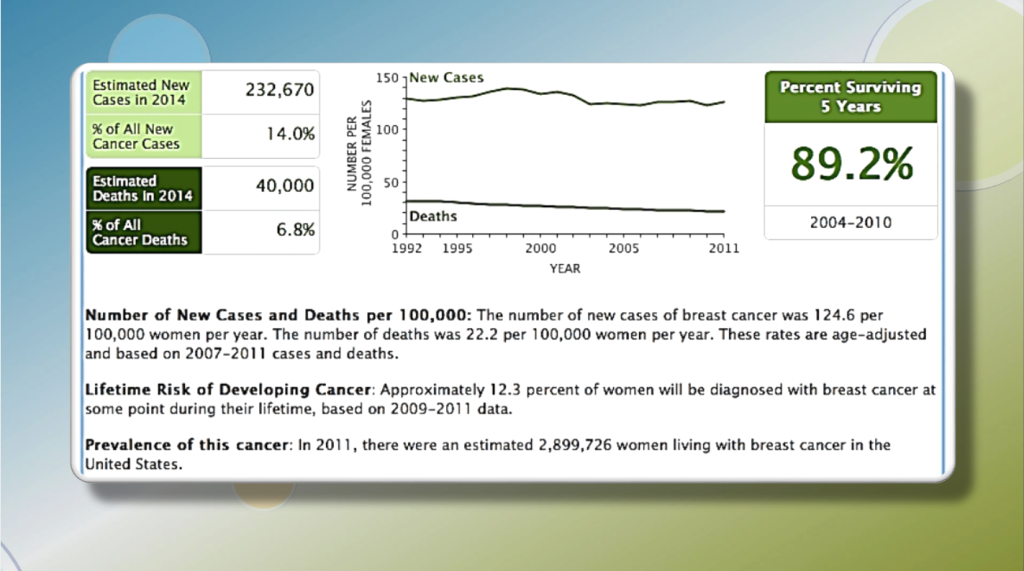
- Does NOT prevent Breast Cancer (only provides earlier detection at best)
- Is no better than Physical Breast Exam at finding Breast Cancer
- OVER DIAGNOSES Breast Cancer in 15-25% of Women screened (35,000 to 58,000 women every year)
- CAUSES DNA MUTATIONS and rapid AGING (a woman ages 4 years every time she gets a Mammogram)
- EMITS IONIZING RADIATION (leading to 10,000 to 20,000 cases of Breast Cancer every year)
- CAUSES DEATHS (estimated to cause 1700 to 3400 deaths every year)
The scientific evidence from decades of multiple Clinical Studies and Meta-Analyses clearly shows that Mammography and its ionizing radiation has the following fatal flaws:
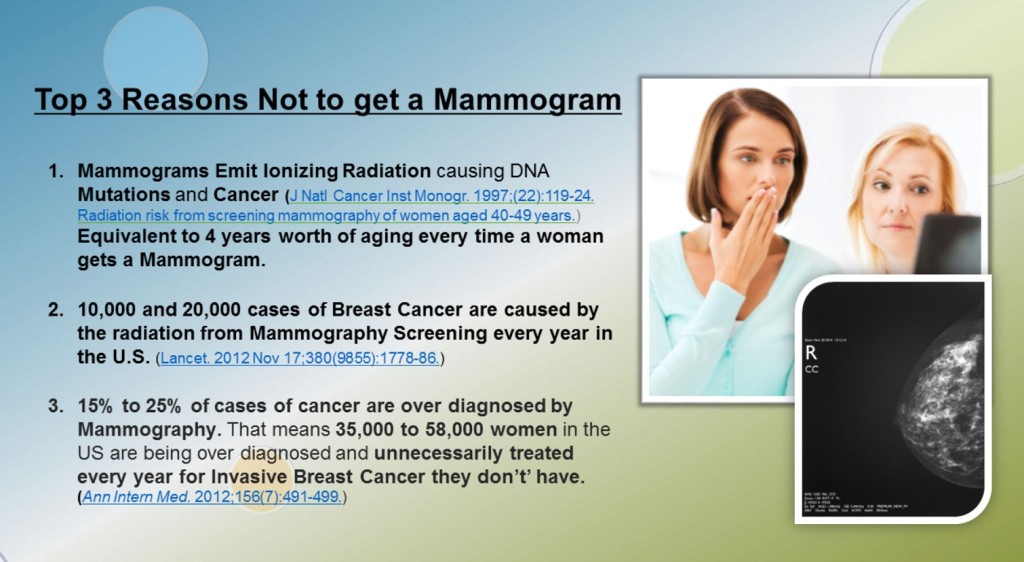
Flaw #1: Mammograms Emit Ionizing Radiation that causes DNA Mutations and Cancer
According to the 2012 Independent UK Panel on Breast Cancer Screening, commissioned by the Cancer Research UK and the Department of Health:
“For every 10,000 women who have regular 3 yearly screenings (Mammogram screens are given only every 3 years in the UK) between the ages of 47 and 73, experts estimate that there will be between 3 and 6 extra breast cancers caused by radiation.” That sounds like a small number, but when that number is multiplied by the 39 million women who get a mammogram each year in the U.S., that equals 10,000 to 20,000 cases of radiation induced Breast Cancer caused by Mammography Screening every year.
The National Cancer Institute estimates that annual mammography of 100,000 women for 10 consecutive years beginning at age 40 would result in up to eight radiation-induced breast cancer deaths. (J Natl Cancer Inst Monogr. 1997;(22):119-24. Radiation risk from screening mammography of women aged 40-49 years.)
Eight deaths out of 100,000 women doesn’t sound like too many, unless of course it is you or someone you love. However, extending that rate to the 39 million women who get a mammogram every year in the U.S., means that at least 3,120 women will die from the annual Mammograms that are supposed to save their life.
Women deserve to know that Mammography exposes them to considerable risk of death over their lifetime. The earlier a woman begins getting mammograms the higher her risk. Sadly women are not being warned of this risk. Dr. David Brenner, with the Center for Radiological Research at Columbia University, says that the real number may be much higher than estimated. Dr. Brenner says that younger women have more cells that are actively dividing, making them even more vulnerable to radiation’s effects than women over the age of 50.
How Many Women Actually Get Cancer from Mammograms?
According to calculations by Dr. David Brenner, professor of radiation oncology and public health at Columbia University, mammography is likely responsible for as many as 6,400 radiation induced cancers every year. Dr. Samuel Epstein, a professor of environmental medicine at the University of Illinois at Chicago School of Public Health, argues that the radiation risks of mammography are notoriously underestimated. Mary Helen Barcellos-Hoff, a radiation biologist at Lawrence Berkeley Laboratories in San Francisco, the average American gets about 360 millirems (a unit for measuring absorbed doses of radiation) of radiation annually, from natural background radiation coming from rocks, radon and cosmic rays, as well as man-made sources.”
To help protect women, the Food and Drug Administration limits the amount of radiation that X-rays can deliver to women’s breasts to 300 millirems per film per view, says Kramer. Even with that restriction, Epstein says, women receive too much radiation. Radiologists routinely take two films per breast. Reporting in the International Journal of Health Services, Epstein and coauthors Rosalie Bertell and Barbara Seaman argue that the premenopausal breast is particularly sensitive to radiation. They estimate that every 1000 millirems of radiation exposure increases the risk of breast cancer by 1 percent. The typical mammogram consists of two X-Rays of each breast for a total of 1200 millirems of radiation and many women get much higher doses do to technician error that require extra retakes.
The American Cancer Society says for every 1,000 women in their 40s screened for 10 years, there will be 600 who will be called back for a repeat mammogram for something suspicious, 350 who will get biopsied, and about five will end up with a diagnosis of breast cancer. And some women might get treated for a cancer that would never have caused a problem. Therefore, women who start getting annual mammograms at age 40 would have at least a 12% increased risk of developing breast cancer due to the screening procedure by the time they turn 50. That does not sound like preventive care to me.
Flaw #2: Mammograms cause the equivalent to 4 years worth of aging every time a woman gets one.
Mammography is not really prevention. A woman ages about 4 years every time she gets a mammogram! Radiation causes cellular damage associated with aging and DNA mutations that raise the risk of developing cancer. The more mammograms you get the greater the risk of getting Cancer.
According to good scientific data that is being mostly ignored in this country, women who start getting annual mammograms at age 40 have a 136% increased risk of dying from breast cancer by the time they turn 50 compared to women who don’t get annual mammograms.
Contrary to common assurances, the radiation exposure of Mammography is not trivial. The routine practice of taking two films for each breast amounts to about 600 millirem (6mGy) focused directly on each breast and at least 1200 millirems total. That is equivalent to the amount of radiation a person gets every four years from environmental exposure. Some women get even more due to radiology technician error, false positive mammograms, or x-ray guided imagery used to take a biopsy of a suspected lump. All of these require a woman to come back for more x-rays. The bottom line is that there is no safe dose of x-rays and the DNA damaging effects are cumulative.
Flaw #3: Mammography is not Prevention and does NOT save lives.
The goal of Breast Cancer Screening with mammography using X-ray imaging is to find breast cancer before a lump can be felt. The goal is to treat cancer earlier, when a cure is more likely. Unfortunately, this well intentioned theory has proven to be false. In June 2013, Drs. Gøtzsche and Jørgensen, from the Cochrane Database of Systematic Reviews, examined seven trials that involved 600,000 women in the age range 39 to 74 years who were randomly assigned to receive screening mammograms or not.
The studies which provided the most reliable information showed that screening did not reduce breast cancer mortality. Studies that were potentially more biased (less carefully done) found that screening reduced breast cancer mortality. However, screening will result in some women getting a cancer diagnosis even though their cancer would not have led to death or sickness. Currently, it is not possible to tell which women these are, and they are therefore likely to have breasts or lumps removed and to receive radiotherapy unnecessarily.
For every 2000 women invited for screening throughout 10 years, one will avoid dying of breast cancer and 10 healthy women, who would not have been diagnosed if there had not been screening, will be treated unnecessarily. Furthermore, more than 200 women will experience important psychological distress including anxiety and uncertainty for years because of false positive findings.
Flaw #4: Mammography leads to over diagnosis and over treatment.
Mammography is unable to differentiate progressive from non-progressive cancers and therefore, results in the overdiagnosis and over treatment of breast cancer.
In the Canadian National Screening Study, 22% of the women diagnosed with invasive breast cancers by Mammography were over-diagnosed, meaning the Mammogram found small, non-progressive lesions that would never have caused them any harm or reduced their life expectancy if left undetected and untreated. The study found that 1 out of every 424 women getting a Mammogram was over-diagnosed, leading to the unnecessary treatment of at least 50,000 women every year, with lumpectomies, mastectomies, chemotherapy and radiation that they did not need. (British Medical Journal BMJ 2014;348:g366)
In July of 2015, a study of 16 million women published in JAMA Internal Medicine by Dr. Richard Wilson and colleagues concluded that mammography leads to a significant overdiagnosis because it is “identifying small, indolent or regressive tumors that would not otherwise become clinically apparent,” and are not true cancers, which means that many women unnecessarily receive disfiguring, harmful and expensive lumpectomies, mastectomies, chemotherapy and radiation treatments they do not need.
Although earlier clinical trials indicated that mammography was effective at detecting small breast cancers early in their progression, Dr. Wilson and his colleagues point out that most of these previous trials are decades old. We have now learned that Mammography has been finding small “non-progressive” tumors that are not true cancers at all and should never have been found or treated. “There are concerns that the benefits and harms may have changed as treatments improved and screening was applied in general practice,” he explains.
Unnecessary treatments from false positives and overdiagnosis adds an additional $4 billion dollars to the cost of care in the U.S. and an unmeasurable amount of anguish and immune suppression due to the stress caused by the fear and worries surrounding such a diagnosis and its prolonged treatment.
In April 2012, Dr. Mette Kalager, M.D., lead author of the Norwegian study entitled, “Overdiagnosis of invasive breast cancer due to mammography screening: results from the Norwegian screening program,” found that for every 2,500 women screened by Mammography, 2,470 to 2,474 will never be diagnosed with breast cancer and 2,499 will never die from breast cancer. Only one death from breast cancer will be prevented, but 6 to 10 women will be overdiagnosed, and treated with surgery, radiation therapy, and possibly chemotherapy without any benefit.
The Norwegian study results found that, “15% to 25% of cases of cancer are overdiagnosed, translating to 6 to 10 women overdiagnosed for every 2500 women invited for screening.” That may not sound like very many, but that translates to 35,000 to 58,000 women out of 230,000 diagnosed with breast cancer in the US who are being overdiagnosed and unnecessarily treated every year for Invasive Breast Cancer that they don’t have.
Flaw #5: Mammography causes 1700-3400 Deaths annually in the US due to the cumulative effects of Radiation exposure.
According to the 2012 Independent UK Panel on Breast Cancer Screening, commissioned by the Cancer Research UK and the Department of Health:
“For every 10,000 women who have regular 3 yearly screenings (Mammogram screens are given only every 3 years in the UK) between the ages of 47 and 73, experts estimate that there will be between 3 and 6 extra breast cancers caused by radiation.” That sounds like a small number, but when that number is multiplied by the 39 million women who get a mammogram each year in the U.S., that equals 10,000 to 20,000 cases of radiation induced Breast Cancer caused by Mammography Screening every year.
The debate should be over. Women should be told to stop getting annual Mammograms!
All of these studies taken together have added powerful new statistical data that refutes the long-held, but false assumption that Mammography would reduce the death rate from Breast Cancer by finding cancer sooner when it is smaller and easier to treat. That assumption has now been proven to be false.
These studies show that the death rates from breast cancer are not reduced by increased Mammogram screening and that Mammography does not reduce the death rate from breast cancer any more than getting a physical breast examination by a trained Physician, but instead leads to overdiagnosis, added expense, anxiety, needless surgeries, chemotherapy and radiation.
So, why would the conventional medical establishment continue recommending annual Mammograms in this country? Could it be that they cannot see that the harm outweighs the benefits, or are they are just unwilling to admit that the harm outweighs the benefits for monetary or liability reasons.
Currently, nearly 75% of all women in the United States age 40 and over get an annual mammogram due to aggressive physician and media pressure and promotion. According to the FDA, 39 million mammograms are performed annually, which at the national median cost per mammogram of $243, is a whopping total of $9.4 Billion dollars.
Ignorance or Bias: Medical, Legal, or Financial?
Unsurprisingly, doctors, especially Radiologists, have come out with an unusually strong pushback against this latest research, as they have consistently done against all research that counters their position. Radiologists, who perform and or interpret Mammograms, have a serious legal liability and monetary vested interest in continuing to recommend annual Mammograms and perhaps they just don’t want to admit that they have been wrong all of these years.
Curiously, the American Cancer Society recommends that “Women should be told about the benefits and limitations linked with yearly mammograms,” yet nowhere on their website do they list or explain any of the risks associated with getting annual Mammograms.
A Step in the Right Direction, but Not Far Enough
In 2009, the U.S. Preventive Services Task Force (USPSTF) recommendation against Mammograms caused a stir when it changed long-held breast-cancer-screening recommendations and advised women to wait until age 50 rather than 40 to start getting mammograms. The task force also said women should only do it every other year, rather than annually and women under age 50 were told that the choice to get mammograms at their age was an individual one. Unfortunately this recommendation was rejected out of hand without due consideration by the medical establishment because it would have looked like rationing in 2009 when Obama Care was being rammed through Congress.
In 2025, the U.S. Preventive Services Task Force (USPSTF) recommends the following:
Women at average risk for breast cancer have a screening mammogram every two years, starting at age 40 and continuing through age 74. This updated guideline was issued in April 2024 and applies to cisgender women and other individuals assigned female at birth. High-risk individuals, such as those with genetic markers or a family history of breast cancer, should discuss personalized screening with their doctor.
-
Earlier Start:
The USPSTF previously recommended that women make an individual decision with their doctor about when to start screening, typically between ages 40 and 50. The new recommendation shifts this to a universal starting age of 40 for everyone at average risk.
-
Increased Inclusivity:The new guidelines are more inclusive of diverse populations and aim to save more lives by promoting earlier screening.
Only the Swiss Medical Board was brave enough to do the right thing and stop Mammography Screening altogether
Based on the now irrefutable evidence against Mammography that has accumulated over the past 25+ years, the Swiss Medical Board has stopped mammography Screening altogether. Are they braver, smarter, or just less concerned about the possible liability associated with potential lawsuits from admitting that the radiation from Mammography causes Breast Cancer in 10,000 to 20,000 women every year and the over diagnosis of cancers that affects another 50,000 women costs an extra $4 billion dollars annually?
First, the Swiss Medical Board observed that the debate about Mammography Screening “was based on a series of reanalyses of the same, predominantly outdated trials.” The Board was concerned that the “modest” benefit of screening might not even be found today because modern breast cancer treatment has “dramatically improved” the prognosis of breast cancer patients. Second, they were concerned that the extremely slim risk reduction in breast cancer mortality that is cited by “most expert panels” comes at the price of a considerable overdiagnosis and unnecessary treatments. Third, they were “disconcerted by the discrepancy between women’s perceptions of the benefits of mammography screening and the benefits to be expected in reality” creates “overly optimistic” expectations of the public about screening, which, in turn, impairs a woman’s ability to make an “informed decision.”
The Swiss Medical Board, in their final report that rejected widespread systematic screening, also recommended that when mammography screening is offered to individual women, a balanced review of harms and benefits be presented.
In the end, Dr. Biller-Andorno, Dr. Jüni, and the rest of the Swiss Medical panel concluded that the benefits of screening do not clearly outweigh the harms, citing an additional analysis from Gilbert Welch, MD, a U.S. expert from Dartmouth College in Hanover, New Hampshire (JAMA Intern Med. 2014;174:448-454).
Unfortunately, none of the major medical institutions in the U.S. are giving women all of the facts or the essential information they need to make an informed decisions. Most say that they feel pressured and pushed to comply.
Why is it that women are not given all the critical facts
The UK Panel, chaired by Sir Michael Marmot, professor of epidemiology and public health and Director of the Institute of Health Equity at University College, London, concluded,“
“It is now vital to give women information that is clear and accessible before they go for a Mammogram so they can understand both the potential harms and benefits of the process.”
First Do No Harm!
The first promise taken by all doctors in the Hippocratic Oath is, “First, do no harm.” Why are women not being told that the very procedure that is being proclaimed as the Preventive measure that can save their life could actually kill them? Women deserve to know the truth. To withhold this information is either negligence, malpractice or fraud.
Women are Scared and Confused
Does this story sound familiar? “I have just gone through a long breast cancer scare the last couple of months, writes a woman who goes by “coffeelatte” on a popular woman’s health blog, “but I was extremely lucky in that the lumpectomy revealed my mass was not a cancer.” “However, I was terrified for more than three months and I am wondering if the fear was worth it and also if the radiation from mammograms is safe or is it another source of problems?” “I ask this because my suspicious mass was back against the breast wall so the radiologist had a very hard time finding the right area to target the wire for the excisional biopsy.
In all, it took her over one hour and I had 12 mammogram pictures before she found the right spot for the wire.” “I am just so upset because I feel if I didn’t have the cancer this time, I sure will the next from all the radiation they are exposing me to. Is this unrealistic of me?” “I feel I try so hard to take care of myself but I end up with problems from the medical care part. I also have a huge, sore incision and scar which is a constant reminder of this miserable ordeal. “Do you ladies think it is best to continue with these mammograms? I just am so confused.” (posted by “coffeelatte” July 2009)
What Should You Do Instead of getting a Mammogram?
 Dr. Gavin T. Royle and colleagues from the Southampton Breast Unit studied diagnostic data for 350 women with suspected breast cancer. Presenting their findings to the 7th Nottingham International Breast Cancer Conference, Royle’s group said that mammography was up to one-third less likely to detect lumps than were physicians. However, mammography was much more effective in determining whether lumps were benign or malignant. (Eur J Cancer 2001 Sep;37 Suppl 5:1-48) General practitioners (GPs) successfully identified lumps in 78% of cases, while breast surgeons were found to be slightly better with an 82% success rate. Mammography only proved sensitive in 63% of patients. “Both GP and breast surgeon clinical examination were more sensitive than mammography in determining if a lump was present,” Royle told conference participants.
Dr. Gavin T. Royle and colleagues from the Southampton Breast Unit studied diagnostic data for 350 women with suspected breast cancer. Presenting their findings to the 7th Nottingham International Breast Cancer Conference, Royle’s group said that mammography was up to one-third less likely to detect lumps than were physicians. However, mammography was much more effective in determining whether lumps were benign or malignant. (Eur J Cancer 2001 Sep;37 Suppl 5:1-48) General practitioners (GPs) successfully identified lumps in 78% of cases, while breast surgeons were found to be slightly better with an 82% success rate. Mammography only proved sensitive in 63% of patients. “Both GP and breast surgeon clinical examination were more sensitive than mammography in determining if a lump was present,” Royle told conference participants.
The study also found that ultrasound, which emits no radiation, was the best noninvasive way of determining whether lumps were benign or malignant. Instead of a Mammogram, get a physical breast exam by the same physician every year. If he or she finds a suspicious lump, get an Ultrasound. If the lump is found on Ultrasound to be hollow in the center, then it is a cyst. If it is solid in the center, then you should get an MRI.
If the MRI is positive then you will need to get a biopsy. If you decide you want to get mammograms, you would be wise to follow the US Preventive Services Task Force recommendations: don’t get a mammogram until age 50, then only get a screening mammogram (only 2 views per breast) every other year until age 74, then don’t get any more.
Hormonal Balance is the key to Breast Cancer Prevention
Excess Estradiol / Deficient Progesterone / Low Estriol
Estradiol is the principal estrogen found in both men and women. A small amount is necessary for optimal function. However, too much Estradiol is associated with causing cancer of the breast, uterus and prostate. Estradiol is fed to beef cows in the U.S. to make them put on more weight so that they can get them to market sooner and sell for more money. Estradiol is also concentrated in milk due to modern dairy farming techniques designed to boost milk production, including feeding cows hormones and milking pregnant cows until very late in their pregnancy. Unfortunately, the trade-off we suffer is a higher rate of Estrogen induced disease, including cancer, which is not recognized or at least not admitted by the Dairy and Beef Industry.
Estrogenic Compounds in Plastics Linked to PMS and Breast Cancer
Polyethylene terephthalate (PETE), the main ingredient in the plastic bottles most widely used for water, sodas, fruit juices, sports drinks, ketchup, mayonaise, peanut butter, vinegar and just about every other food you can think of, has been found to leach harmful estrogenic chemicals into the bottles’ contents. Known as phthalates, these chemicals have now been linked to the disruption of both male and female hormones and may be a significant reason for the dramatic increase in PMS, uterine fibroids, endometriosis and cancer. To learn more about how PETE plastics may affect your health, click here and watch this video.
Estriol is the Safe, Protective Estrogen
Estriol is known as the weak estrogen because it is 1000 times weaker than Estradiol. However, it is found in high livels in women during pregnancy and while breast feeding. It is believed to be the reason for the 7% decreased risk of breast cancer for each pregnancy and the 4.3% decreased risk for each 12 months of breastfeeding. Estriol is found in high quantities in women without breast cancer and low levels in women with breast cancer. It is known to block the harmful effects of Estrone and Estradiol on breast tissue. It is 1000 times less stimulating to breast and uterine tissue than Estradiol. When it is found in a woman in sufficient quantities it will bind to breast tissue and prevent cancer by blocking Estrone and Estradiol.
Compared to women who had never used HRT, taking Bio-Identical Estriol alone produced a 30% reduced risk of breast cancer. Estriol selectively binds to estrogen receptor-beta (ER-beta), which inhibits breast cell proliferation and prevents breast cancer development. (Source: Postgraduate medicine, Vol 121, Issue 1, January 2009; Endocrinology. 2006 Sep;147(9):4132-50. Epub 2006 May 25.)
Progesterone Provides Powerful Cancer Prevention
A deficiency of Progesterone in women and/or an excess of Estradiol is associated with PMS, uterine fibroids, endometriosis and Osteoporosis, as well as Breast, Ovarian and Uterine Cancer. Progesterone is the natural counter-balance to Estradiol. Progesterone activates Tumor Suppressor Protein (p53), known as the “guardian of the cell,” suppress excessive cell growth that can lead to cancer. Progesterone also decreases the cancer activating protein known as bcl-2. The researchers found “a maximal 90 percent inhibition of cell proliferation with T47-D breast cancer cells after exposure to 10 microM progesterone for 72 hours. (Ann Clin Lab Sci.1998 Nov-Dec;28(6):360-9.)
Tumor Suppressor Protein p53 guards against cellular mutations that can cause cancer in the following ways:
- Activation of DNA repair
- Stops Cell growth when necessary to allow DNA time to repair
- Initiates programmed cell death (apoptosis) when DNA damage is irreparable
Estradiol Promotes Cancer
Estradiol, on the other hand, does the opposite of progesterone. It causes a decrease in p53 and activates bcl-2, the opposite acting protein that promotes cancer cell growth. Breast cancer cells do not multiply when women have a sufficient supply of Estriol and Progesterone.
(Source: Ann Clin Lab Sci. 1998 Nov-Dec;28(6):360-9; Int J Cancer. 2003 Jul 10;105(5):607-12)
PREVENTION SUMMARY
Dr. Hansen Rx for Breast Cancer Prevention:
1. Don’t get routine mammograms; Get a breast exam from the same physician every year. If a lump is found get an Ultrasound; If the lump is hollow its a cyst and no further testing is needed. If the lump is solid then get an MRI, which is more sensitive than a Mammogram. If after all this information, you still feel that you want to get mammograms, I suggest you only follow the minimal recommendation of the US Preventive Services Task Force: don’t get a mammogram until age 50, then only get a screening mammogram (only 2 views per breast) every other year until age 74, then don’t get any more.
2. Avoid synthetic estrogens, in Birth Control Drugs, hormone replacement therapy (HRT), plastics and pesticides and especially glyphosate made by Monsanto.
3. Eat a Healthy diet: 2 fruits daily (especially flavonoid-rich fruits like grapes, blueberries, plums, cherries and cranberries that destroy cancer cells; 3 vegetables daily (include broccoli regularly because it sweeps the harmful estrogens (estrone and estradiol) out of the body; 4 grains; eat meat sparingly; avoid saturated fats, especially estrogen fed beef and dairy products; eat soy regularly because it contains a plant estrogen that is identical to Estriol, the body’s cancer preventing estrogen.
4. Take Peak Advantage – High Potency Multi-Vitamin with 20x the RDA for B Vitamins, including Folic acid; antioxidants (including Vitamin A, Beta-Carotene, C, & E, plus GSE Ultra 110 Grape Seed Extract a potent anti-cancer bioflavonoid, that helps cells recognize and destroy Cancer and blocks excessive production of Estrone and Estradiol within the Breasts by inhibiting excessive Aromatase activity that is known to be increased in women with Breast Cancer)
5. Test your hormones annually and take natural, bio-identical, plant derived Estriol and Progesterone to balance your hormones and help prevent cancer.